Introduction: A series of 78 laparoscopic hernioplasties performed in the General Teaching Hospital “Enrique Cabrera”.
Objective: To determine perioperative events, surgical complications and the evaluation of the pain referred by the operated
patients.
Methods: Between January 2012 and December 2018, 78
hernioplasties were performed laparoscopic in 60 patients; 18 had
bilateral inguinales hernias. He collected the variables: age, sex, type
of hernia, perioperative events and complications, and a pain
scale was applied. A database was filled and processed statistically.
Results: The male sex predominated in a 5:1 ratio, the
surgical time average was 53.5 minutes for unilateral hernias and 71.3
minutes for the bilateral ones. The most frequent complication in the
transoperative period was bleeding lower in 27.0%, and in the
postoperative period the hematoma was in 15.3%, it recurred two hernias
(2.5%). At 15 days after surgery, 93.3% of theoperated
did not complain of pain, but the social and labor reintegration was of
only 34% of patients.
Conclusion: laparoscopic inguinal hernioplasty is a therapeutic option more, mainly in patients with bilateral and reproduced
hernias.
Keywords:Laparoscopic Hernioplasty; Inguinal Hernia; Hernia Recurrence
Introduction
Since the concept of endoscopic inguinal hernia repair was first
described by Ger R [1] in 1982, the endoscopic techniques are gone
modifying, going through a time when failures and complications
-united to high cost-exceeded initial enthusiasm [2]. Laparoscopic
hernioplasty (HL) has been gaining popularity in the last decade,
and numerous controlled studies appear in the literature comparing
the laparoscopic techniques with conventional techniques [3-7]. In
recent years, HL, despite consolidated as a therapeutic option to
consider. The advantages of this have been demonstrated method
in bilateral hernias, relapsed and in the active labor subject, that
requires a precocious labor reintegration [5-7].
Methods
Between June 2012 and June 2018, a prospective descriptive
study of Longitudinal section of 60 patients operated by hernia
endoscopy of the region inguinal, in the Department of Surgery of the
General Teaching Hospital “Enrique Cabrera”. The inclusion criteria
were: - Patients who agreed with the type of surgical intervention
and the study, and They gave their informed consent. Patients
older than 30 years classified ASA I-III, without contraindications
anesthetics for laparoscopic interventions.
a) Patients classified as Nyhus III and IV. Exclusion criteria.
b) Patients with previous surgical wounds in the inguinal
region to operate, not dependent on inguinal hernias
reproduced.
c) Inguinal hernias complicated, irreducible or slipped.
The surgical techniques were: laparoscopic inguinal
hernioplasty completely extraperitoneal (TEP) of total extraperitoneal
English and inguinal hernioplasty laparoscopic
transabdominal preperitoneum (TAPP) preperitoneal), and
one or the other was performed, at the discretion of the main
surgeon. The TEP technique was executed with some variants
such as: not using the trocar balloon, the preperitoneal space was
decoloured by means of the 0º laparoscope, and the insufflation
of CO2 at 13 mmHg. In patients with large herniated rings, placed
a polypropylene cone in the hernia defect and then a 15 x 12 cm
polypropylene prosthesis. There was no need to fix with clips the
tights. The TAPP technique was performed on a regular basis [8].
In the immediate postoperative period, the scale of visual pain
analog scale was applied (VAS), [9] and a value was assigned to pain
through “caritas”, which starts very cheerful (value I) until very sad
(value X). The quantification of pain was repeated in consultation at
7, 15 days and one month after surgery.
Results
There were operated 78 hernias in 60 patients (18 patients
[30.0%] suffered from bilateral hernias, 69 primary hernias and
9 reproduced hernias). The average of age was 55.6 years, the
youngest patient was 30 years and the oldest was 77 years, but the
majority (12 patients) were in the fifth decade of life. The male sex
predominated in 82.9%, which represented a relationship man /
woman of 5: 1. 42.9% of patients performed large efforts habitual
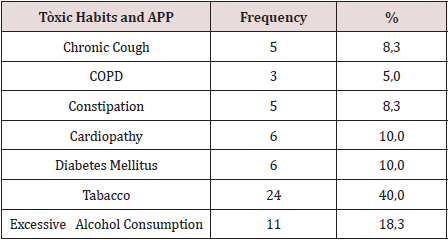
physicists. The pathological history of the patients (Table 1). It is
observed that 24 patients (40.0%) consumed tobacco, and in 11
an excessive consumption of alcohol was collected 18.3%. COPD:
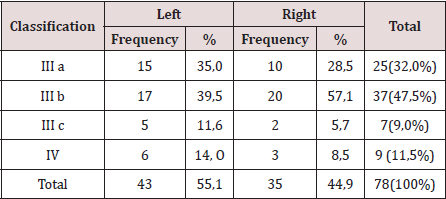
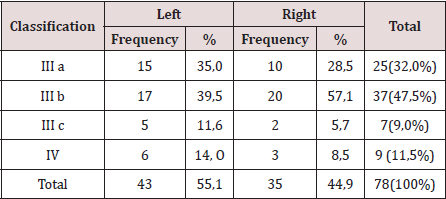
Chronic Obstructive Pulmonary Disease (Table 2). The distribution
of the series according to the Nyhus classification. Right hernias
predominated (55.1%), the indirect variety with large dilation of
the ring and destruction of the posterior wall (IIIb) was the most
frequent (37 hernias), and 7 femorales hernias and 9 recurrent
hernias were operated 73 PET (93.6%) and 5 TAPP (6.4%) were
performed. Two of the patients in whom a TEP technique was
started were converted to a conventional prosthetic technique by
accidental perforation of the peritoneum, passing the CO2 into the
peritoneal cavity, and consequently, the loss of the preperitoneal
surgical space. Of the 5 TAPP repairs, 3 of them were in the course
of a laparoscopic cholecystectomy, and another was the conversion
of a failed PET technique. The average surgical time of unilateral
hernias was 53.5 min, with a minimum of 25 min and a maximum
of 120 min. In bilateral repairs, the average surgical time was 71.3
min, and a minimum of 40 and a maximum was observed. of 110
minutes.
Table 1: Toxicos habits, and personal phalogical history (APP).
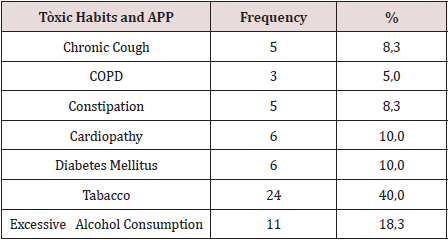
Table 2: Distribution According to the Nyhus Classification.
The hospital stay was less than 24 h in 50 patients (71.4%), in
5 it extended from 24 to 48 h, and in 5 to more than 48 hours. The
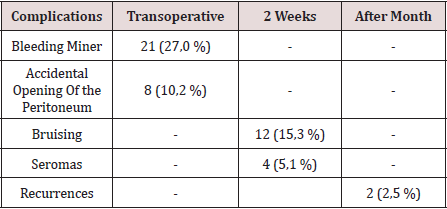
most frequent complication in the transoperative period (Table
3) was minor bleeding in 21 repairs (27.0%) that gave rise to 12
hematomas (15.3%). No complications were observed after the
second week, but two patients suffered recurrences (2.5%), more
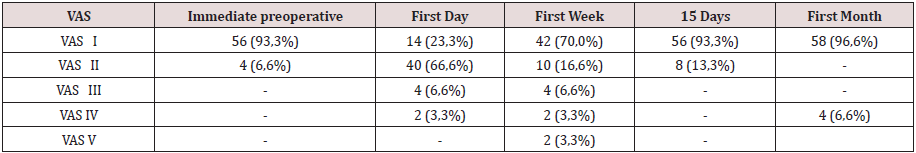
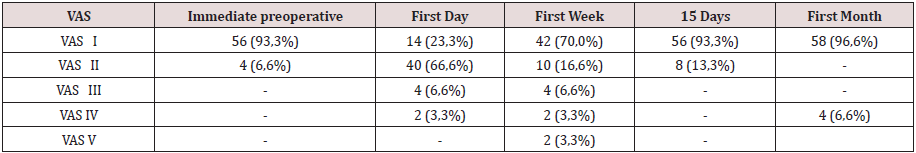
than two months after surgery. The application and evaluation of
the VAS scale (Table 4). In the immediate postoperative period,
after the patient recovered from anesthesia, 56 individuals (93.3%)
were classified as VAS I, and 4 as VAS II. Twenty-four hours after
surgery, 14 patients (23.3%) were classified as VAS I, 40 (66.6%) as
VASII, 4 patients as VAS III and 2 VAS IV. In the consultation of the
first week of postoperatively, 42 patients (70.0%) were classified
as VAS I and [10] as VAS II, and two patients with moderate pain
(VAS V) appeared in this period. Fifteen days after surgery, 56
individuals (93.3%) were VAS I and a month were 58 (96.6%). The
incorporation to the usual activities, including work, was 3 patients
a week after surgery, at 15 days they were 19 patients (31.6%) and
54 patients a month (90.0%).
Table 3: Complications.
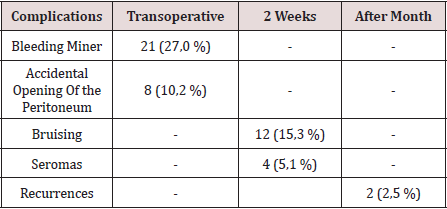
Table 4: Evaluation of the Visual Analogy Scale (VAS).
Discussion
Currently, with the improvement of laparoscopic techniques,
these are outlined as safe, reproducible and as a therapeutic option
regardless of the age of the patient; nevertheless, the evaluation of
the individual must be correct and meticulous in the preoperative
period, specifically cardiorespiratory function, since with the TEP
method a working space is created between the sheets of the crosssection
sheet, richly vascularized, so that absorption and elimination
of CO2 is greater than that produced in the peritoneal cavity during
the performance of the pneumoperitoneum [10]. Although men
predominated, there was a slight increase in women in the series
with respect to other authors, [3-5] which could have been due to
the inclusion in the study of 3 women who underwent the diagnosis
of inguinal hernia, in the course of a laparoscopic cholecystectomy.
In laparoscopic practice, it is not uncommon finding of hernia
defects diagnosed in the transoperative, in men and women, the
latter basically with a history of gynecological disorders. Although
the usefulness of hernia repairs in asymptomatic patients is
questioned in some articles, [11,12] the authors consider that it
would be beneficial for the patient, if conditions permit, the repair
of the hernia defect by the TAPP method. The relationship between
the hernia disease and the physical efforts, is classic from the
Cooper era [1]. In the series, 68% of the patients performed physical
activities involving large and medium efforts, and also analyzing
the multifactorial character in the pathogenesis of hernia disease,
was striking, that approximately half of the patients operated on
were smokers, a factor that influences the metabolism of collagen,
significantly linked to hernia recurrences [13]. The majority of the
repairs were by means of the PET technique, and we consider, as
other authors [10,14 -19], that although the TAPP technique brings
us closer to the area from a family perspective to the surgeon
(peritoneal cavity) and facilitates the so-called “learning curve”, the
hernial disease - considering it a parietal defect- should be given
solution from this same plane to avoid the likelihood of serious
complications of intrabdominal , and to leave the transperitoneal
method as a tactical resource when the totally extraperitoneal
method is unsuccessful.
The average surgical time was similar to other series [3-6].
It is known that this tends to decrease when the surgical team
gains experience [16]. The largest surgical time recorded was in a
patient, who was started with a PET technique, but Due to technical
difficulties, it was converted to a conventional posterior repair. The
fundamental complications were in relation to minor bleeding in the
transoperative period and postoperative hematomas. In 3 patients
it was necessary to drain the hematoma due to the discomfort
caused, however, in the rest of the patients with hematomas and
seromas they were treated with conservative measures. In two
patients, the recurrence occurred 2 months after surgery, which
was interpreted as a technical error. Our results coincide with
numerous studies [3-7], that indicate the least postoperative pain
of the minimum access techniques, as well as a prompt social and
labor reincorporation of the patients. Despite the fact that 70%
and 93.3% a week and 15 days postoperatively, respectively, had
no pain or discomfort were minimal, only [18] individuals (30%)
were incorporated into their usual activities before 15 days. These
results contrast with other studies that report a return to work and
social activities between 10-15 postoperative days, 4-17- although
it is likely that some sociocultural factors are influencing these
results. It can be concluded by noting that laparoscopic inguinal
hernioplasty is another therapeutic option, mainly in patients with
bilateral and reproduced hernias. In the series there were no major
transoperative or postoperative complications, only minor bleeding
and bruising were present. Most patients were not afflicted by
pain 2 weeks postoperatively, however, return to social and labor
activities after 15 days was low [18-20].
Read More Lupine Publishers Surgery and Case Studies Journal Articles: https://surgery-casestudies-lupine-publishers.blogspot.com/