Thursday, October 31, 2019
Lupine Publishers: Lupine Publishers-Environmental Issues and Disaste...
Lupine Publishers: Lupine Publishers-Environmental Issues and Disaste...: Lupine Publishers- Environmental and Soil Science Journal What is Environment and Why it is Important? This is a vas...
Wednesday, October 30, 2019
Lupine Publishers: Intellectual Irrigation Management in Mining Froze...
Lupine Publishers: Intellectual Irrigation Management in Mining Froze...: Lupine Publishers- Environmental and Soil Science Journal Abstract This article examines the current state of soil and ...
Tuesday, October 29, 2019
Lupine Publishers: Lupine Publishers | Creative Process in the Design...
Lupine Publishers: Lupine Publishers | Creative Process in the Design...: Lupine Publishers | Journal of Textile and Fashion Designing Introduction Creative process Man has his creative manifest...
Friday, October 25, 2019
Lupine Pubishers| Cervical Spinal Cord Injury During Coronary Artery Bypass Graft Surgery in An Elderly: A Case Report
Lupine Publishers | Journal of Surgery & Case Studies
Intraoperative spinal cord injury (SCI) is uncommon and the
pathology has not cleared. We report cervical cord injury without
vertebral fracture during a coronary artery bypass operation.
Cervical cord compression (CCC) is compression of the cervical
spinal cord that occurs during the normal course of aging and
may progress into cervical spondylotic myelopathy (CSM), which
can cause neurologic dysfunction. Many people with cervical
cord compression are asymptomatic. However, patients with CCC
are at higher risk of SCI following minor injury. An 85-year-old
woman with asymptomatic cervical cord compression underwent
a coronary artery bypass graft surgery. After the surgery, he
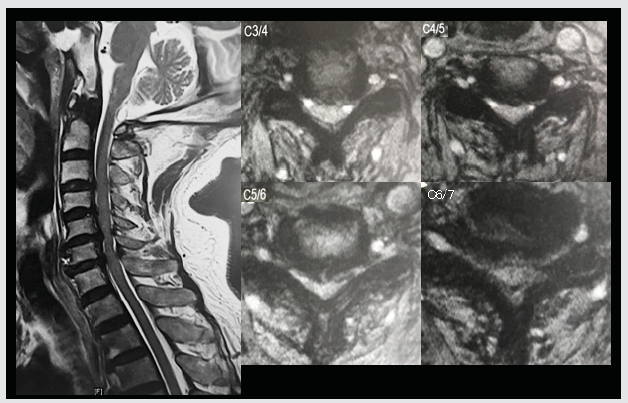
developed tetraplegia. MRI revealed severe spinal cord compression
from C3 to C7 and C5/6 signal change of spinal cord (Figure 1). The
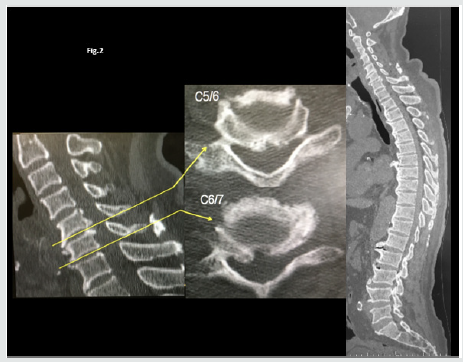
radiograph and CT showed diffuse idiopathic skeletal hyperostosis
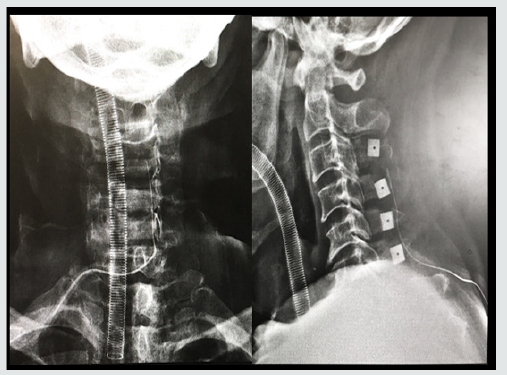
and thoracic kyphosis of 55 degree (Figure 2). Cervical SCI after
was diagnosed. After the diagnosis, we underwent laminoplasty
(Figure 3). And he almost completely recovered after surgery.
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
Case Report
Figure 3: The radiograph and CT showed diffuse idiopathic skeletal hyperostosis and thoracic kyphosis Radiograph after
laminoplasty for cervical spinal cord injury.
Iatrogenic cervical SCI after non spinal surgeries that
requires neck hyperextension is rarely reported, probably due
to underdiagnosis and underreport. In the current aging society,
the prevalence of patients with CCC is expected to increase. In
our population-based magnetic resonance imaging (MRI) study,
the prevalence rate of CCC was 24.4%, and it was higher with
increasing age in both men and women [1]. Among the 15 cases
(including ours) published in the literature [2], most patients had
cervical cord compression and were old men. Eight patients had
undergone coronary artery bypass surgery that requires prolonged
operative time. Only 3 patients had almost complete recovery.
Two patients required tracheostomy for long-term ventilator
support. Two patients died. These cases reiterate the potential risk
of iatrogenic SCI in people with predisposing conditions such as
cervical spondylosis and CCC. Moreover, in this case, the patient had
diffuse idiopathic skeletal hyperostosis and thoracic kyphosis of
55 degree, which can lead inflexibility of spine. The inflexibility of
thoracic spine might cause hyperextension of cervical spine during
the surgery. Surgeries requiring prolonged neck hyperextension
put patients with cervical spondylosis and CCC at risk for SCI. It is
essential to recognize the potential occurrence of iatrogenic SCI
might endanger patients’ lives.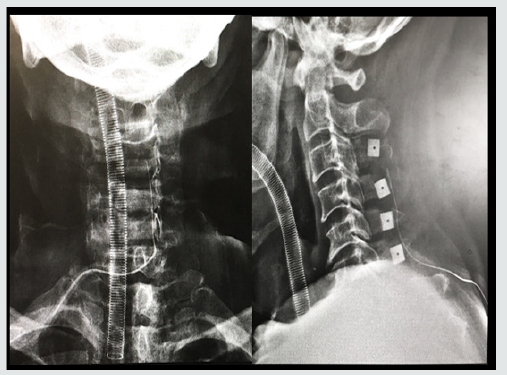
For more Lupine Publishers Open Access Journals Please visit our website:
For more Surgery Journal articles Please Click Here:
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Twitter : https://twitter.com/lupine_online
Lupine Publishers: Lupine Publishers | On A Criminal Trace of Crippli...
Lupine Publishers: Lupine Publishers | On A Criminal Trace of Crippli...: Lupine Publishers | Journal of Orthopaedics Case Report In 2010, the Czech Republic participated in the World Health Organ...
Thursday, October 24, 2019
Lupine Publishers: Lupine Publishers | Future Prospect for Sustainabl...
Lupine Publishers: Lupine Publishers | Future Prospect for Sustainabl...: Lupine Publishers | Journal of Textile and Fashion Designing Abstract The treasure of Major natural fibres belongs to cotton...
Wednesday, October 23, 2019
Lupine Publishers: Lupine Publishers | Some Significant Advances in Y...
Lupine Publishers: Lupine Publishers | Some Significant Advances in Y...: Lupine Publishers | Journal of Textile and Fashion Designing Abstract The article reviews some of the significant researches i...
Tuesday, October 22, 2019
Lupine Publishers: The Most Perfect Ecosystem: The Qanat Karez Salt L...
Lupine Publishers: The Most Perfect Ecosystem: The Qanat Karez Salt L...: Lupine Publishers- Environmental and Soil Science Journal Abstract More than 150,000 Gallerias, Qanat Karez sweet wat...
Monday, October 21, 2019
Lupine Publishers: Lupine Publishers | On A Criminal Trace of Crippli...
Lupine Publishers: Lupine Publishers | On A Criminal Trace of Crippli...: Lupine Publishers | Journal of Orthopaedics Case Report In 2010, the Czech Republic participated in the World Health Organiz...
Thursday, October 17, 2019
Lupine Publishers: A Mechanics-Based Procedure for Predicting Groundw...
Lupine Publishers: A Mechanics-Based Procedure for Predicting Groundw...: Lupine Publishers- Environmental and Soil Science Journal Abstract A procedure for predicting cumulative slope displace...
Wednesday, October 16, 2019
Lupine Publishers: Haiwan (Malay Version)
Lupine Publishers: Haiwan (Malay Version): Lupine Publishers- Environmental and Soil Science Journal Opinion Translated by Fuzaini Sahar, through this book young childr...
Monday, October 14, 2019
Lupine Publishers: Lupine Publisher | The Definition Technological Pa...
Lupine Publishers: Lupine Publisher | The Definition Technological Pa...: Lupine Publishers | Journal of Textile and Fashion Designing Abstract In article it is showed the definition technological ...
Saturday, October 12, 2019
Lupine Publishers | All-On-Four Treatment Concept in Dental Implants: A Review Articles
Lupine Publishers | Journal of Surgery & Case Studies
Edentulism has been demonstrated to have negative social and
psychological effects on individuals that include adverse impacts
on facial and oral esthetics, masticatory function and speech abilities,
that when combined, are translated into significant reductions
in patients’ quality of lives. It is well-known that immediate placement
of implants is a challenging surgical procedure that requires
proper treatment planning and surgical techniques. There are several
prosthetic options to rehabilitate severely atrophic maxillae
and mandibles have been developed such as conventional complete
dentures, implant supported removable and implant supported
fixed prosthesis. Implant supported prosthesis may not be feasible in
many conditions because of the vicinity of vital anatomical
structures, poor bone quality and quantity.
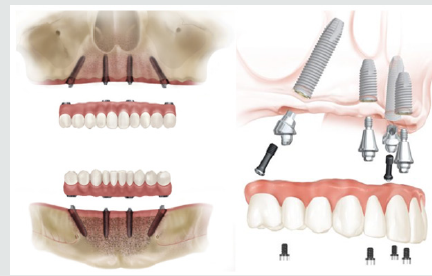
The implant technology developed as the all-on-four concept is offered as an alternative to conventional implant applications. In the all-on-four technique, 4 implants are placed in the inter foraminal region in the mandible and in the pre-maxillary region in total edentulism cases. An exception is the all-on- Four concept, which uses only 4 implants to support an acrylic, screw-retained provisional prosthesis delivered on the day of implant placement, followed by a definitive prosthesis approximately 4 months later. The patient can also be benefited with the immediate rehabilitation of edentulous arches which helps maintaining self-confidence and quality of life.
Keywords: All on four concept; Dental implant; Tilted implant; Severe atrophy
Abbreviation: CT: Computerized Tomography; Ncm: Newton centimeter ; mm: Millimeter
One of the greatest challenges in implant dentistry is the
treatment of patients with severely atrophic jaws. Such atrophy
can be horizontal or vertical or both; even if sufficient vertical bone
is present, lack of ridge width can still preclude treatment with
implants that are 4 mm in diameter or wider. Over the years, many
techniques, procedures, and materials have been introduced to
solve the complex problems associated with treatment of atrophic
jaws. One early approach in the posterior maxilla was to augment
the sinus in conjunction with the simultaneous placement of
implants [1–3]. In cases where the mandibular bone height is less
than 12.0 mm, tissue augmenting techniques including bone ridge
expansion and bone grafts are typically made necessary to allow
the placement of traditional dental implants. Despite their widespread
use, these techniques are clinically very challenging and
display higher levels of tissue and implant morbidity.
Modern oral rehabilitation strategies based on the utilization of dental implants and immediate loading techniques, have been demonstrated to allow for the rapid and efficient restoration of patients with superior esthetic and masticatory properties, while reducing the morbidity and damage to both soft and hard tissues. In some cases of the completely edentulous patients, implant supported prosthesis treatment is almost impossible without complex techniques such as nerve transposition and grafting in the posterior maxilla and mandible. A solution for such situations is the All-on-4 concept [4]. Implant supported prosthesis may not be feasible in many conditions because of the vicinity of vital anatomical structures like mandibular canal or maxillary sinus. Over the years, many techniques, procedures, and materials have been introduced to solve the complex problems associated with treatment of atrophic jaws and avoid the vicinity of vital anatomical structures such as the use of short implants, alveolar distraction osteogenesis, guided bone generation, use of intraoral and extraoral autogenous bone grafts, nerve repositioning etc. The high cost, time and morbidity associated with such approaches have limited their application.
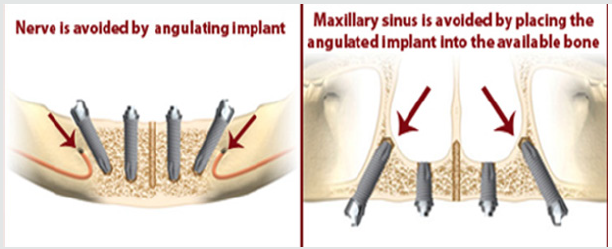
At the beginning of the millennium, distally tilted implants were proposed, enabling the use of denser bone located in the anterior mandible for improving bone anchorage, and replacement of posterior teeth without extended cantilevers and avoiding bone grafting procedure [5]. The “all-on-four” treatment concept was developed to maximize the use of available remnant bone in atrophic jaws, allowing immediate function and avoiding regenerative procedures that increase the treatment costs and patient morbidity, as well as the complications inherent to these procedures [6].
One of the early designs of the All-on-4 style concept can be
traced back to Mattson and colleagues, in 1999 whereby they treated,
patients with severely resorbed edentulous maxilla by inserting
4 to 6 implants in the premaxilla to avoid sinus augmentation
and successfully restored them with fixed prosthesis with 12
teeth supported by superstructure [7]. In 2000, Krekmanov and
colleagues were also able to demonstrate posterior tilted implantsupported
prosthesis was possible. The All-on-4 immediate loading
concept was developed, institutionalized and systematically
analyzed in the 2003 by a dentist Paulo Malo and colleagues [8].
This concept uses 2 vertical anterior implants in conjunction with
2 distally tilted inclined implants with their apices positioned
anterior to the sinus wall or mental foramen (Figure 1). It involves
the use of straight and angled multiunit abutments, which support
a provisional, fixed, and immediately loaded, full arch prosthesis.
It has been developed to maximize the use of available bone and
allows immediate function [9] (Figure 2).
In this technique, four implants are placed in the anterior region of the jaw between the two mental foramina in the mandible and between the mesial walls of the maxillary sinus in the maxilla. The two anterior implants follow the jaw anatomy and the two distal implants are tilted at 45° angulation (Figure 1). Many longterm studies and published data on the All-on-4 concept reported cumulative survival rates between 92.2% and 100% [10].
a. Maximize the use of available bone
b. To allow for Immediate Function.
b. No severe parafunctions
c. To diminish the cantilever, tilt the posterior implants.
d. Does not require a wider opening of the mouth
e. It is advisable to place implants between extraction sockets.
f. Indicated with a minimum bone width of 5mm and minimum
bone height of 10mm from canine to canine in maxilla and 8mm in mandible. g. If angulation is 300 or more, the tilted implants can be splinted. For tilted posterior implants, the distal screw access holes should be located at the occlusal face of the first molar, the second premolar, or the first premolar.
II. Less invasive procedure for the pt.
III. Graft less procedure.
IV. Implants well-spaced, good biomechanics, easier to clean, immediate function and aesthetics
V. Simplified surgical & prosthetic procedure.
VI. Reduced cost due to less number of implants.
VII. High success rates.
VIII. Angled posterior implants:-
a. Avoid anatomical structures
b. Allow longer implants anchored in better quality bone
c. Reduces posterior cantilever
b. Free hand arbitrary surgical placement of implant is not always possible as implant placement is completely prosthetically driven.
c. It is very technique sensitive and requires elaborate presurgical preparation such as CAD/CAM, surgical splint [11].
I. Surgical Protocol
II. Prosthetic Phase
I. Step 1: Selection of case satisfying the inclusion criteria
II. Step 2: Planning implant placement using All-On-4 Guide (Prefered)
III. Step 3: Location of Maxillary Antrum and Mental Foramen with All-On-4 Guide
IV. Step 4: Implant placement done following the protocols
The surgical guide is placed into a 2 mm osteotomy that is made in the midline position of the maxilla or mandible and the titanium band is contoured to follow the arc of the opposing arch. The mandibular guide also assists in retracting the tongue. The vertical lines on the guide are used as a reference for drilling at the correct angulation, which should not be greater than 45º. Angulated pins and denture can also be used as templates. The two most anterior implants follow jaw anatomy in direction (lingual tilting in cases of severe mandibular resorption). The two posterior implants are inserted just anterior to the foramina or maxillary sinus and tilted distally approximately 30°– 45° relative to the occlusal plane. Implant torque is set to greater than 35 Ncm. If the torque values for three or more implants are below 35 Ncm, a 2-stage technique is preferred [9].
A recent shift in practice paradigm has been to minimize
treatment costs and patient morbidity while providing the most
satisfying patient-centered treatment outcomes according to the
state of the art of dental practice. The “All on-Four” treatment
concept is an attempt to reach these objectives by providing
relatively straight forward, predictable treatment option to
rehabilitate edentulous patients with a high outcome of Quality
of life [13]. Babbush et al. described a protocol of combining the
3.5-mm-diameter Nobel Active implants with the All-on-4 concept
and reported on the results of 227 implants after 1 to 3 years of
Follow-up. The cumulative survival rate was 98.7% at the end of
3 years, with a 100% prosthetic survival rate [14]. Paul Malo did
retrospective clinical studies and found that long-term outcomes
( up to 10 years ) of 245 patients with completely edentulous
mandibles rehabilitated with the All-on-4 treatment concept and
reported cumulative implant survival rates of 93.8% and 94.8%
using the patient and implant as units of analysis, respectively [15]
Lopes et al. did a prospective study to evaluate the medium- and
long-term outcomes of the rehabilitation of completely edentulous
jaws in immediate function with the All-on-4 treatment concept
using a computer-guided surgical protocol and reported an
overall 96.6% cumulative survival rate after 5 years of follow-up
[16]. Published studies on the All on-Four concept have shown
cumulative survival rates to range between 92.2% and l00% [10].
clinical research over the past decade has shown that more than 4
dental implants to support a full, fixed (non-removable) bridge is
typically not necessary, and that placing more than 4 implants does
not increase success rates[17]. Owing to the freedom of tilting, the
implants can be anchored in dense bone structures (anterior bone
with higher density) and well spread anteriorly-posteriorly giving
an effective prosthetic base. By reducing the number of implants
to four, each implant can be placed without coming into conflict
with adjacent implants. This treatment approach, using tilting and
few implants rather than inserting several implants competing for
space, has demonstrated good results.
The “All-on-4” treatment concept seems to be an alternative
option for rehabilitating edentulous jaws compared with advanced
surgical approaches without using removable prostheses. It is
a cost-effective procedure, decreasing the treatment times, the
morbidity and allowing a higher patient quality of life. Placement
of dental implants previously in attempts to treat the severely
resorbed maxilla and mandible has had only limited success. But
the rehabilitation of completely edentulous, atrophied maxilla
and mandible by the placement of implants using the AII-on-Four
protocol gives new hope for a perceivable success, while becoming
a promising treatment method of choice and standard in the care
for severely compromised patients.
Abstract
The implant technology developed as the all-on-four concept is offered as an alternative to conventional implant applications. In the all-on-four technique, 4 implants are placed in the inter foraminal region in the mandible and in the pre-maxillary region in total edentulism cases. An exception is the all-on- Four concept, which uses only 4 implants to support an acrylic, screw-retained provisional prosthesis delivered on the day of implant placement, followed by a definitive prosthesis approximately 4 months later. The patient can also be benefited with the immediate rehabilitation of edentulous arches which helps maintaining self-confidence and quality of life.
Keywords: All on four concept; Dental implant; Tilted implant; Severe atrophy
Abbreviation: CT: Computerized Tomography; Ncm: Newton centimeter ; mm: Millimeter
Introduction
Modern oral rehabilitation strategies based on the utilization of dental implants and immediate loading techniques, have been demonstrated to allow for the rapid and efficient restoration of patients with superior esthetic and masticatory properties, while reducing the morbidity and damage to both soft and hard tissues. In some cases of the completely edentulous patients, implant supported prosthesis treatment is almost impossible without complex techniques such as nerve transposition and grafting in the posterior maxilla and mandible. A solution for such situations is the All-on-4 concept [4]. Implant supported prosthesis may not be feasible in many conditions because of the vicinity of vital anatomical structures like mandibular canal or maxillary sinus. Over the years, many techniques, procedures, and materials have been introduced to solve the complex problems associated with treatment of atrophic jaws and avoid the vicinity of vital anatomical structures such as the use of short implants, alveolar distraction osteogenesis, guided bone generation, use of intraoral and extraoral autogenous bone grafts, nerve repositioning etc. The high cost, time and morbidity associated with such approaches have limited their application.
At the beginning of the millennium, distally tilted implants were proposed, enabling the use of denser bone located in the anterior mandible for improving bone anchorage, and replacement of posterior teeth without extended cantilevers and avoiding bone grafting procedure [5]. The “all-on-four” treatment concept was developed to maximize the use of available remnant bone in atrophic jaws, allowing immediate function and avoiding regenerative procedures that increase the treatment costs and patient morbidity, as well as the complications inherent to these procedures [6].
History of the All-on-4® concept
In this technique, four implants are placed in the anterior region of the jaw between the two mental foramina in the mandible and between the mesial walls of the maxillary sinus in the maxilla. The two anterior implants follow the jaw anatomy and the two distal implants are tilted at 45° angulation (Figure 1). Many longterm studies and published data on the All-on-4 concept reported cumulative survival rates between 92.2% and 100% [10].
Treatment Planning
The All-on-4 clinical solution has been developed toa. Maximize the use of available bone
b. To allow for Immediate Function.
General Considerations
a. Ability to achieve primary implant stability (35 – 45 Ncm)b. No severe parafunctions
c. To diminish the cantilever, tilt the posterior implants.
d. Does not require a wider opening of the mouth
e. It is advisable to place implants between extraction sockets.
f. Indicated with a minimum bone width of 5mm and minimum
bone height of 10mm from canine to canine in maxilla and 8mm in mandible. g. If angulation is 300 or more, the tilted implants can be splinted. For tilted posterior implants, the distal screw access holes should be located at the occlusal face of the first molar, the second premolar, or the first premolar.
Advantages of the All-on-4 Concept
I. Avoids complex surgery,II. Less invasive procedure for the pt.
III. Graft less procedure.
IV. Implants well-spaced, good biomechanics, easier to clean, immediate function and aesthetics
V. Simplified surgical & prosthetic procedure.
VI. Reduced cost due to less number of implants.
VII. High success rates.
VIII. Angled posterior implants:-
a. Avoid anatomical structures
b. Allow longer implants anchored in better quality bone
c. Reduces posterior cantilever
Disadvantages
a. Length of cantilever in the prosthesis cannot be extended beyond the limit.b. Free hand arbitrary surgical placement of implant is not always possible as implant placement is completely prosthetically driven.
c. It is very technique sensitive and requires elaborate presurgical preparation such as CAD/CAM, surgical splint [11].
Treatment Protocol Consists of Two Phases: Surgical and Prosthetic
II. Prosthetic Phase
I. Step 1: Selection of case satisfying the inclusion criteria
II. Step 2: Planning implant placement using All-On-4 Guide (Prefered)
III. Step 3: Location of Maxillary Antrum and Mental Foramen with All-On-4 Guide
IV. Step 4: Implant placement done following the protocols
The surgical guide is placed into a 2 mm osteotomy that is made in the midline position of the maxilla or mandible and the titanium band is contoured to follow the arc of the opposing arch. The mandibular guide also assists in retracting the tongue. The vertical lines on the guide are used as a reference for drilling at the correct angulation, which should not be greater than 45º. Angulated pins and denture can also be used as templates. The two most anterior implants follow jaw anatomy in direction (lingual tilting in cases of severe mandibular resorption). The two posterior implants are inserted just anterior to the foramina or maxillary sinus and tilted distally approximately 30°– 45° relative to the occlusal plane. Implant torque is set to greater than 35 Ncm. If the torque values for three or more implants are below 35 Ncm, a 2-stage technique is preferred [9].
Prosthetic Phase
17º multiunit abutments and 30º angulated, Straight Abutments with different collar heights are placed onto the implants. These are used to achieve the correct access allowing relative parallelism and so that the rigid prosthesis can be seated passively [12]. For provisional prosthesis fabrication on the day of surgery (2–3 hours after surgery), the impression copings are placed onto the multiunit abutments which are then splinted with autopolymerising resin and wire bars. It ensures an accurate transfer without accidental displacement of the impression copings and impression is made. Protective healing caps are placed on the abutments while provisional is being made. Acrylic provisional screw retained prosthesis is torqued to 15 Ncm. Only soft diet is recommended. For final prosthesis (4–6 months after initial implant placement), if the implants are judged stable, provisional restoration is removed and bite is registered. Multiunit laboratory analogs are attached to the provisional and then it is mounted on an articulator against a counter model. The prosthesis is indexed with putty. Resin pattern is fabricated in sections and the sections are joined in the patient’s mouth. This resin pattern gets scanned and framework is made by CAD/CAM technology. After try-in of the framework, final prosthesis is fabricated and delivered. Final prosthesis can be a metal-acrylic resin with a titanium framework and acrylic resin prosthetic teeth, or a metal ceramic prosthesis with titanium framework and all ceramic zirconia crowns [12].Discusión
Conclusion
For more Lupine Publishers Open Access Journals Please visit our website:
For more Surgery Journal articles Please Click Here:
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
Follow on Twitter : https://twitter.com/lupine_online
Friday, October 11, 2019
Lupine Publishers: Lupine Publishers | A Combined Material Substituti...
Lupine Publishers: Lupine Publishers | A Combined Material Substituti...: Lupine Publishers | Journal of Textile and Fashion Designing Abstract This paper empirically presents a batik production pro...
Thursday, October 10, 2019
Lupine Publishers: Panduan Penternakan Burung Puyuh (Malay Version)
Lupine Publishers: Panduan Penternakan Burung Puyuh (Malay Version): Lupine Publishers- Environmental and Soil Science Journal Opinion Written by Jabatan Perkhidmatan Veterinar Neg...
Wednesday, October 9, 2019
Lupine Publishers: Lupine Publishers | An Infrared Technique for Rapi...
Lupine Publishers: Lupine Publishers | An Infrared Technique for Rapi...: Lupine Publishers | Journal of Textile and Fashion Designing Abstract An infrared technique used to analyze pineapple leaf f...
Lupine Publishers: Lupine Publishers | The Role Effectiveness of Phys...
Lupine Publishers: Lupine Publishers | The Role Effectiveness of Phys...: Lupine Publishers | Journal of Orthopaedics Abstract Today, the emergence and growth of mental disorders are more noticea...
Friday, October 4, 2019
Lupine Publishers: Lupine Publishers | The Role Effectiveness of Phys...
Lupine Publishers: Lupine Publishers | The Role Effectiveness of Phys...: Lupine Publishers | Journal of Orthopaedics Abstract Today, the emergence and growth of mental disorders are more noticea...
Thursday, October 3, 2019
Lupine Publishers: Partial Budgeting Analysis of an Intervention of ‘...
Lupine Publishers: Partial Budgeting Analysis of an Intervention of ‘...: Lupine Publishers- Environmental and Soil Science Journal Abstract Reported Impact Assessment of an intervention ‘Land Shap...
Tuesday, October 1, 2019
Lupine Publishers: Breeding population of Terns and Western Reef Hero...
Lupine Publishers: Breeding population of Terns and Western Reef Hero...: Lupine Publishers- Environmental and Soil Science Journal Abstract The research was conducted on Ghabre Nakhoda and Dara islands in ...
Subscribe to:
Posts (Atom)
Gallstone Ileus in the Elderly: Still a Challenge, Report of a Case with Review of the Current Literature
Abstract Introduction: Gallstone ileus is described as an intestinal obstruction caused by luminal gallstone impaction. It is a mainly ...
-
Intellectual Corruption at the APA by James F. Welles in Surgery & Case Studies: Open Access Journal in Lupinepublishers A book...
-
Acute Liver Failure and Thyrotoxicosis Managed with Liver Transplant and Thyroidectomy by Gerardo Tamayo Enriquez in Surgery & Ca...
-
Lupine Publishers | Journal of Surgery & Case Studies Abstract From 1963 to 2019 7,600 ...