Lupine Publishders | Journal Of Surgery & Case Studies
Background
Symptomatic mesenteric ischaemia is an uncommon disease entity which
can prove complicated to diagnose and manage. Both
endovascular and open operative approaches have been described but the
nutritional complications caused by poor gut absorption
can mean that these patients may be at higher risk of operative
complications, and appropriate care should be given to preoperative
nutritional optimisation prior to surgical management.
Keywords: Critical Mesenteric Ischaemia; Iron Supplementation; Preoperative Optimisation
Chronic mesenteric ischaemia (CMI) caused by atherosclerotic
stenosis of the arteries supplying the small bowel is a fairly
common finding at autopsy (reported to be between 12-60% of
elderly patients at autopsy [1]), however symptomatic critical
mesenteric ischaemia is rarely reported and can elude diagnosis
for extended periods of time due to the non-specific symptoms of
presentation. Patients may complain of post-prandial abdominal
pain, appetite and weight loss, and “food fear” [2]. In these patients,
as the disease process can be protracted and well-established by
time of diagnosis and management, patients may show signs of
long-term undernourishment, including weight loss, electrolyte
and micronutrient deficiencies and declining overall health [3]. As
such, substantial preoperative optimisation may be required prior
to consideration of operative management and revascularisation.
Consideration should also be given postoperatively to a possibility
of re-feeding syndrome. We present here the case of a 70-yearold
woman seen in our unit with a complex critical mesenteric
ischaemia compounded with general frailty and undernourishment.
A 70-year-old woman was initially referred by her primary care
doctor for assessment of unintentional weight loss for investigation
of possible malignancy. At time of referral, the patient had lost 9
kilograms (from 51kg to 42kg) within 4 months (body mass index
18) and complained of persistent nausea and upper abdominal
pain. She was noted to have a background of rheumatoid arthritis
and chronic obstructive pulmonary disease. A CT scan of the thorax,
abdomen and pelvis did not show any sign of malignant lesions, and
upper gastrointestinal endoscopy revealed only mild gastritis. The
patient was treated with helicobacter pylori eradication therapy
and discharged (Figure 1). She was re-referred to the service
following further concerning weight loss to a body weight of 35kg
with a BMI of 12.86. A repeat upper GI endoscopy was completely
normal. Blood tests showed a mild red cell macrocytosis (MCV 100)
and low ferritin levels; renal function, electrolytes and liver function
tests were unremarkable. Further review of CT imaging revealed an
occluded coeliac trunk with stenosis at the origin of the superior
mesenteric artery and suspicion of post-stenotic aneurysm.
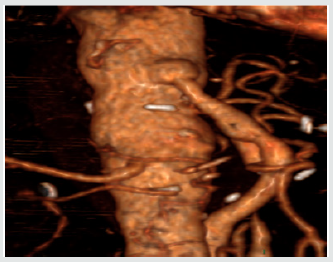
The patient underwent CT angiography which showed critical stenosis with short occlusion of the coeliac trunk origin, and a 3cm occlusion at the origin of the superior mesenteric artery. Bowel was entirely supplied by collateral vessels originating from the inferior mesenteric artery, which was itself also stenosed at its origin. Abdominal aorta, renal arteries and iliac vessels did not show any significant disease. Attempts were made to treat the stenoses with an endovascular approach but were ultimately unsuccessful as it was not possible to identify mesenteric vessel origins due to severity of stenosis. Following this the patient was planned to undergo supracoeliac aortic-SMA bypass, with preoperative optimisation with IV iron supplementation. The patient’s low ferritin levels at diagnosis were supplemented by this approach and came up to normal levels by the time of procedure; this was reflected in the improved full blood count of the patient.” The patient underwent laparotomy and adhesiolysis, following which the root of the SMA was identified (Figures 2 & 3).
ACritical mesenteric ischaemia poses a particular challenge for
preoperative optimization; reduced arterial supply of the small
bowel is likely to affect its function and the degree to which this
occurs is likely to depend on the severity of the stenotic areas.
Equally, preoperative anaemia is known to increase the risk of blood
transfusion, and in turn, increase the morbidity and mortality risk
of undergoing a procedure [4]. A recent study involving patients
with colorectal cancer treated with preoperative intravenous
iron supplementation showed that the haemoglobin level was
significantly increased in the active treatment group, however
the further impact of this increase on risk levels of morbidity
and mortality is not known [5]. In particular, the effectiveness of
this intervention is unknown in patients undergoing high risk
aortic surgery. A 2015 Cochrane report identified 3 prospective
randomised controlled trials investigating its use – two in colorectal
surgery and one gynaecological study. This review suggested that
there was a reduction in use of blood transfusions associated with
preoperative intravenous iron supplementation but it was not
statistically significant. Each of these studies had small patient
numbers, however, and overall the authors note that the studies
are unlikely to have had sufficient power to reliably analyse the
significance of the effect [6].
We present a case of critical mesenteric ischaemia with use
of preoperative intravenous iron supplementation. Intravenous
iron replacement therapy has been noted in the literature to have
reduced the prevalence of preoperative anaemia, though more
studies are needed to see if this truly translates to lower levels of
operative morbidity and mortality, and if this effect is seen across
differing surgical procedures.
Abstract
Background
Symptomatic mesenteric ischaemia is an uncommon disease entity which
can prove complicated to diagnose and manage. Both
endovascular and open operative approaches have been described but the
nutritional complications caused by poor gut absorption
can mean that these patients may be at higher risk of operative
complications, and appropriate care should be given to preoperative
nutritional optimisation prior to surgical management.
Objective
We present a case of critical mesenteric arterial stenosis treated with preoperative intravenous iron supplementation to illustrate preoperative optimisation and therapeutic approaches, together with a selected review of the literature
Conclusion
Preoperative parenteral iron supplementation is likely to be effective in reducing preoperative anaemia but the impact of this intervention on postoperative blood transfusion and other complications in the context of complex aortic surgery is unknown.Keywords: Critical Mesenteric Ischaemia; Iron Supplementation; Preoperative Optimisation
Introduction
Case Report
The patient underwent CT angiography which showed critical stenosis with short occlusion of the coeliac trunk origin, and a 3cm occlusion at the origin of the superior mesenteric artery. Bowel was entirely supplied by collateral vessels originating from the inferior mesenteric artery, which was itself also stenosed at its origin. Abdominal aorta, renal arteries and iliac vessels did not show any significant disease. Attempts were made to treat the stenoses with an endovascular approach but were ultimately unsuccessful as it was not possible to identify mesenteric vessel origins due to severity of stenosis. Following this the patient was planned to undergo supracoeliac aortic-SMA bypass, with preoperative optimisation with IV iron supplementation. The patient’s low ferritin levels at diagnosis were supplemented by this approach and came up to normal levels by the time of procedure; this was reflected in the improved full blood count of the patient.” The patient underwent laparotomy and adhesiolysis, following which the root of the SMA was identified (Figures 2 & 3).
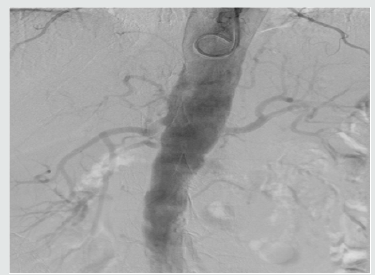
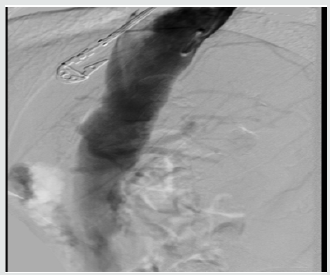
Figure 5: Postoperative CT with 3D reconstruction
showing right renal artery takeoff and vein graft.
A long saphenous vein graft was harvested and anastamosed to
the supracoeliac aorta proximally and the terminal SMA distally. On
completion of anastamosis and upon opening of the graft, the small
bowel became flushed pink and began enthusiastically peristalsing
almost immediately (Figures 4 & 5). Postoperatively the patient
progressed well, and upon follow up, had gained 7kg in the space
of 3 months. Symptoms of post-prandial pain and nausea, as well
as appetite generally, had improved significantly from her previous
morbid state.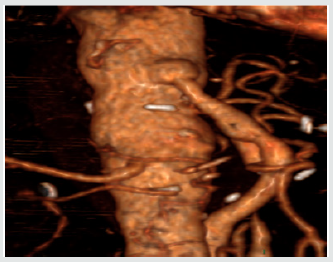
Discussion
Conclusion
For more Lupine Publishers Open Access Journals Please visit our website:
http://www.lupinepublishers.us/
For more Surgery Journal articles Please Click Here:
https://lupinepublishers.com/surgery-case-studies-journal/
http://www.lupinepublishers.us/
For more Surgery Journal articles Please Click Here:
https://lupinepublishers.com/surgery-case-studies-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers



No comments:
Post a Comment